What are the symptoms?

A deeper look: Muscle tone, stretch reflex and spasticity
In simple terms, spasticity is characterised by increased resistance to passive movement and is caused by prolonged muscle contraction.1
Muscle tone is a state of tension that is maintained continuously, even when a person is relaxed, and which increases in resistance to passive stretch.2,3 It helps to maintain posture and decreases during sleep.4,5 The stretch reflex is a muscle contraction in response to stretching within the muscle. This reflex, by definition extremely fast, exists to allow the muscle to adapt to any kind of muscular tone and change to avoid overstretching.6
In spasticity, the muscle tone is abnormally increased (muscle hypertonia) and reflexes, such as the stretch reflex, may persist for too long and may be too strong (hyperactive reflexes).3,7 These phenomena cause an increased resistance to passive movement (e.g. if someone else tries to move the extremities of the person affected).3
Symptoms of spasticity
Spasticity can range from very mild to debilitating and painful.8,9
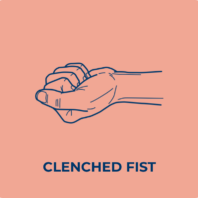
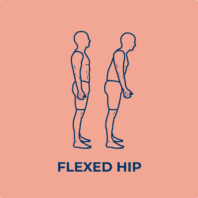
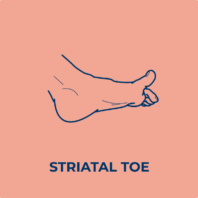
The main symptoms are10:




How does spasticity affect different parts of the body?
Spasticity symptoms can occur in the upper and/or the lower limbs.7 The extent of spasticity and areas of the body affected depend on the area of the brain or spinal cord that has been damaged.12
Spasticity can be associated with hemiplegia, hemiparesis, diplegia and quadriplegia.


Hemiplegia / Hemiparesis
Patients with spasticity and hemiplegia have prolonged muscle contractions1 and severe or complete loss of strength and paralysis on one side of the body.13 Generally, injury to the left side of the brain will cause symptoms in the right side of the body, and vice versa.14
Patients with spasticity and hemiparesis have abnormally stiff muscles and weakness on one side of the body. Patients affected can still move the impaired side of their body but with reduced muscular strength.13
This can be associated with other deficits such as a decrease in sensitivity and/or a reduction in body part position perception. Hemiplegia is more severe and defined as total absence of controlled movement.


Diplegia
In spastic diplegia, the lower limbs are most often affected, and the term used is paraplegia. These cases are mainly related to a lesion of the spinal cord. Diplegia rarely concerns the two upper limbs.15


Quadriplegia
All four limbs are affected in patients with spastic quadriplegia.15
Upper limb spasticity
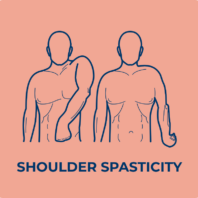
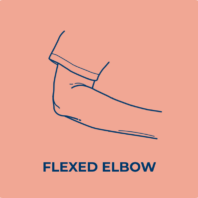
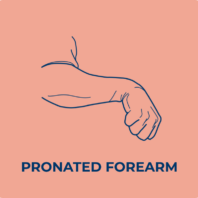
While spasticity may affect any muscle group, it often produces stereotypical patterns in posture. Spasticity frequently affects muscles that work against the force of gravity. In other words, upper limb spasticity tends to affect the flexors (biceps, brachialis and brachioradialis) of the arm.3
When a patient suffers from spasticity, these patterns can all affect their motor ability when performing simple everyday tasks such as dressing, eating or grasping,7 and may also interfere with balance, causing mobility difficulties.11
Common clinical patterns of upper limb spasticity include7:


Lower limb spasticity
Spasticity often produces stereotypical patterns in posture, depending on the muscles affected by increased muscle tone.
Spasticity frequently affects muscles that work against the force of gravity. In other words, in the leg, it tends to affect the extensors.3
Common clinical patterns of lower limb spasticity include7:




References
1Escaldi S, Bianci F, Bavikatte G, Molteni F, Moraleda S, Deltombe T, Francisco G. Module 1: pathophysiology and assessment of spasticity; goal setting. J Int Soc Phys Rehabil Med. 2022 5(Suppl 1):S3-S22. doi: 10.4103/2349-7904.347807.
2Ganguly J, Kulshreshtha D, Almotiri M, Jog M. Muscle tone physiology and abnormalities. Toxins (Basel). 2021 Apr 16;13(4):282. doi: 10.3390/toxins13040282.
3Trompetto C, Marinelli L, Mori L, Pelosin E, Currà A, Molfetta L, Abbruzzese G. Pathophysiology of spasticity: implications for neurorehabilitation. Biomed Res Int. 2014;2014:354906. doi: 10.1155/2014/354906.
4Masi AT, Hannon JC. Human resting muscle tone (HRMT): narrative introduction and modern concepts. J Bodyw Mov Ther. 2008 Oct;12(4):320-32. doi: 10.1016/j.jbmt.2008.05.007.
5Schwarz PB, Yee N, Mir S, Peever JH. Noradrenaline triggers muscle tone by amplifying glutamate-driven excitation of somatic motoneurones in anaesthetized rats. J Physiol. 2008 Dec 1;586(23):5787-802. doi: 10.1113/jphysiol.2008.159392.
6Bhattacharyya KB. The stretch reflex and the contributions of C David Marsden. Ann Indian Acad Neurol. 2017 Jan-Mar;20(1):1-4. doi: 10.4103/0972-2327.199906.
7Thibaut A, Chatelle C, Ziegler E, Bruno MA, Laureys S, Gosseries O. Spasticity after stroke: physiology, assessment and treatment. Brain Inj. 2013;27(10):1093-105. doi: 10.3109/02699052.2013.804202.
8Brainin M. Poststroke spasticity: Treating to the disability. Neurology 2013 Jan 15;80(3 Suppl 2):S1-4. doi: 10.1212/wnl.0b013e3182762379.
9Wissel J, Manack A, Brainin M. Toward an epidemiology of poststroke spasticity. Neurology. 2013 Jan 15;80(3 Suppl 2):S13-9. doi: 10.1212/WNL.0b013e3182762448.
10Royal College of Physicians. Spasticity in adults: management using botulinum toxin. National Guidelines. 2018. Available at: https://archive-rcplondon.zedcloud.co.uk/file/12449/download%202018 [accessed September 2025].
11Marque P, Denis A, Gasq D, Chaleat-Valayer E, Yelnik A, Colin C; Botuloscope Group; Pérennou D. Botuloscope: 1-year follow-up of upper limb post-stroke spasticity treated with botulinum toxin. Ann Phys Rehabil Med. 2019 Jul;62(4):207-213. doi: 10.1016/j.rehab.2019.06.003.
12Sheean G. The pathophysiology of spasticity. Eur J Neurol. 2002 May;9 Suppl 1:3-9; discussion 53-61. doi: 10.1046/j.1468-1331.2002.0090s1003.x.
13Stern LZ, Bernick C. The motor system and gait. In: Walker HK, Hall WD, Hurst JW (editors). Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed. Boston: Butterworths, 1990; 351-355.
14National Institute of Neurological Disorders and Stroke (NINDS). April 2020. Post-stroke rehabilitation. NIH Publication No. 20-NS-4846. National Institutes of Health. Available at: https://catalog.ninds.nih.gov/sites/default/files/publications/post-stroke-rehabilitation.pdf [accessed September 2025].
15Shevell MI. The terms diplegia and quadriplegia should not be abandoned. Dev Med Child Neurol. 2010 Jun;52(6):508-9. doi: 10.1111/j.1469-8749.2009.03566.x.


